《IInnovations and brief communications》
Clip-assisted endoscopic cyanoacrylate injection for gastric varices with a gastrorenal shunt: a multicenter study
Mingyan Zhang*, 1, Ping Li*, 2, Haijun Mou3, Yongjun Shi1, Biguang Tuo3, Suyun Jin1, Ruonan Sun1, Guangchuan Wang1,
Jiali Ma2, Chunqing Zhang1
【1 Department of Gastroenterology and Hepatology,Shandong Provincial Hospital affiliated to Shandong University, Jinan, China
2 Department of Endoscopy, Beijing Ditan Hospital,Beijing, China
3 Department of Gastroenterology, the Affiliated Hospitalof Zunyi Medical College, Zunyi, China】
ABSTRACT:
Background:The aim of this study was to evaluate the safety and efficacy of clip-assisted endoscopic cyanoacrylate injection for gastric varices with a gastrorenal shunt.
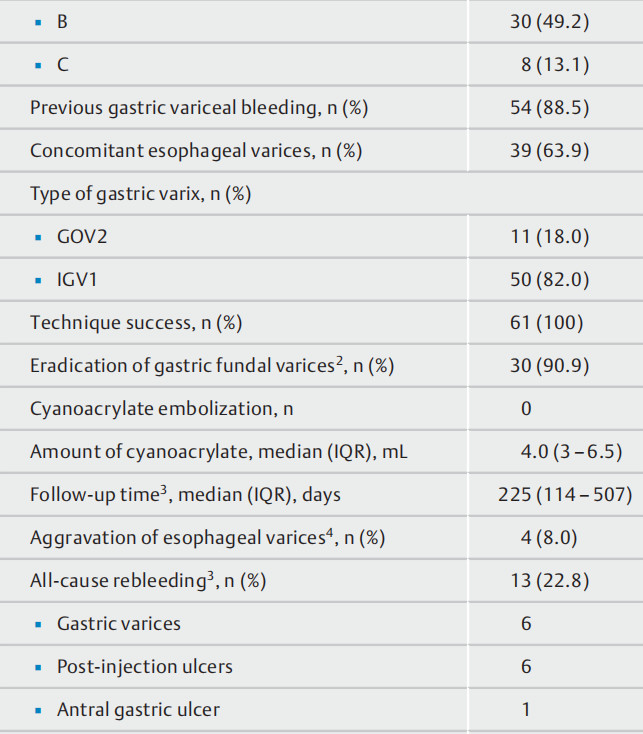
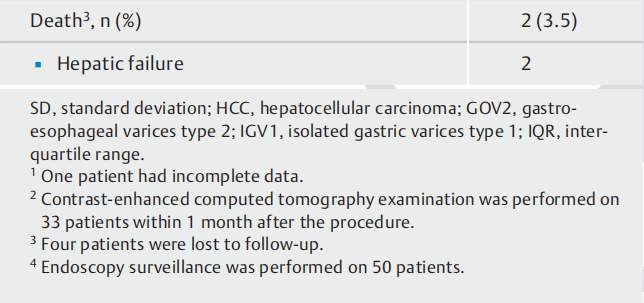
Methods:Records were reviewed of patients with gastric varices and concomitant gastrorenal shunts who underwent clip-assisted endoscopic cyanoacrylate injection at three tertiary centers between April 2016 and October 2018. The assessed outcomes were technical success rate,eradication of gastric varices, cyanoacrylate embolization,and all-cause rebleeding.
Results:A total of 61 patients were analyzed. The procedure was successful in all patients (100 %). Gastric varices were eradicated in 30 of 33 patients (90.9 %) according to contrast-enhanced computed tomography re-examination within 1 month after the procedure. No symptoms or signs of cyanoacrylate embolization related to the procedure were observed. Four patients (6.6 %) were lost to follow-up.All-cause rebleeding occurred in 13/57 patients (22.8 %)during a median follow-up period of 225 days (interquartile range 114 – 507 days).
Conclusions:Clip-assisted endoscopic cyanoacrylate injection appeared to be a safe procedure that was convenient and efficacious in the treatment of gastric varices with concomitant gastrorenal shunt.
Gastric varices, which are observed in approximately 20 % of patients with portal hypertension [1], bleed less frequently than esophageal varices, but bleeding from the former is much more severe when it does occur [2]. Therefore, effective management of such bleeding or prevention of rebleeding is essential. Endoscopic cyanoacrylate injection is the treatment for hemostasis and prevention of gastric variceal rebleeding recommended by the Baveno VI Consensus Workshop [3]. However,severe adverse events related to cyanoacrylate embolization,including pulmonary embolization, splenic infarction, and cere-bral and myocardial infarction, have been reported [4 – 6], raising concerns regarding the safety of cyanoacrylate injection.
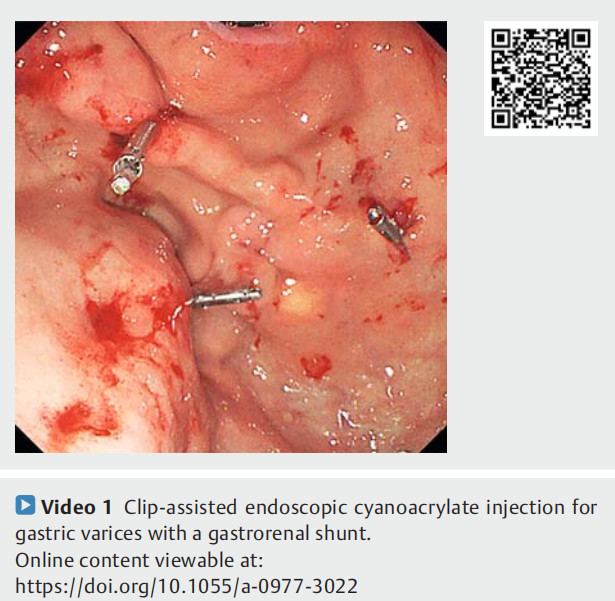
In the present study, the inflow or outflow veins of the gastric varices were first clamped with metal clips to slow down or completely block the gastric variceal blood flow, followed by cyanoacrylate injection into the gastric varices (?Video 1).This novel approach may reduce the risk of ectopic embolization. The results of 61 patients who underwent the procedure at three institutions are reported below.
Methods
Patients
This investigation was a multicenter study of patients with cirrhosis who underwent clip-assisted endoscopic cyanoacrylate injection between April 2016 and October 2018. Patients meeting the following inclusion criteria were analyzed: 1) cirrhosis diagnosed on the basis of clinical, radiological or laboratory parameters, and/or liver biopsy; 2) gastric varices (gastroesophageal varices type 2 [GOV2] and isolated gastric varices type 1 [IGV1]) confirmed by endoscopy; 3) a gastrorenal shunt confirmed by contrast-enhanced computed tomography (CT);and 4) high risk gastric varices, active gastric varices or a history of bleeding attributable to gastric varices. The exclusion criteria were: age < 18 years or > 80 years; regional portal hypertension;a history of previous liver transplantation, transjugular intrahepatic portosystemic shunt or surgical splenectomy combined with variceal devascularization; significant cardiopulmonary comorbidity; the presence of hepatocellular carcinoma not meeting the Milan criteria; and the presence of other malignancies that significantly affect survival. Electronic medical records were reviewed for patient demographic details, etiology of the underlying liver disease, laboratory values, procedural information, and clinical, endoscopic, and imaging follow-up data.
Written informed consent concerning the procedure of clipassisted endoscopic cyanoacrylate injection was obtained from each patient. This was a retrospective study and was approved by the Ethics Committee of Shandong Provincial Hospital.
Procedures
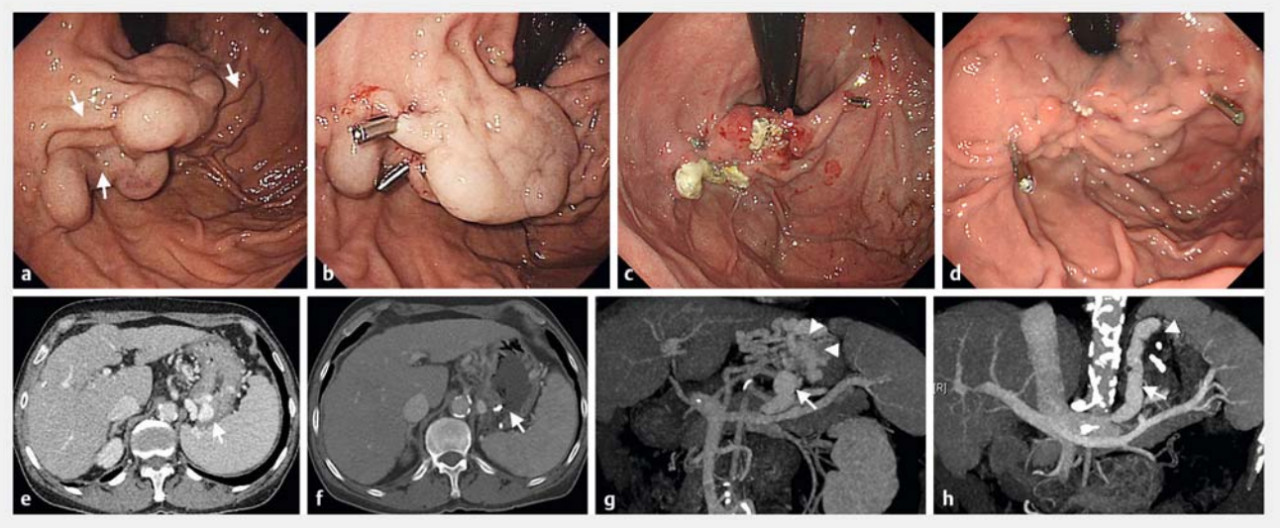
Using the contrast-enhanced CT images, we tried to identify the inflow and outflow veins of the gastric varices under endoscopy. Metal clips were deployed on the inflow or outflow veins to restrict the blood flow within the varices. The clips were placed on the narrow part of the tortuous varices to clamp the whole varices as fully as possible. After the metal clips had been placed, a “modified sandwich method” (lauromacrogol, cyanoacrylate, lauromacrogol) was used to inject the cyanoacrylate into the gastric varices [7]. The needle catheter was used to determine adequate filling of the varices and the need for additional injections (?Fig. 1). Endoscopic band ligation was performed on patients with large esophageal varices after clipassisted endoscopic cyanoacrylate injection. Antibiotic prophylaxis was routinely administered for 24 – 72 hours following the injection.
Follow-up
Telephone follow-ups, clinical follow-ups, medical histories,and records were all used to collect the information. Technical success was defined as the clips being deployed and the cyanoacrylate being injected for adequate filling of the varices. The technical success rate, eradication of gastric varices, cyanoacrylate embolization, aggravation of esophageal varices,and all-cause rebleeding were evaluated.
Statistical analysis
Continuous variables are presented as the mean (standard deviation) if normally distributed and as the median (interquartile range [IQR]) otherwise. Categorical variables are expressed as percentages. Statistical software (SPSS 21.0; IBM Corp., Armonk, New York, USA) was used for statistical analyses.
Results
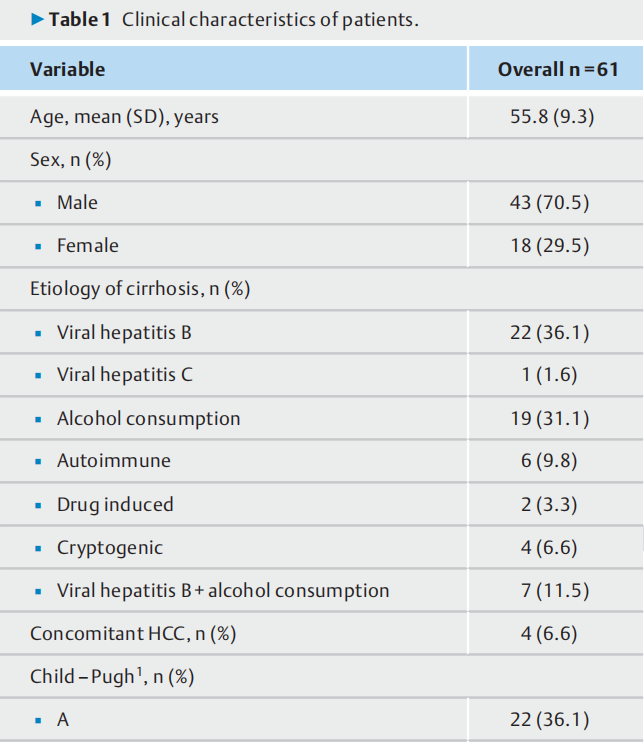
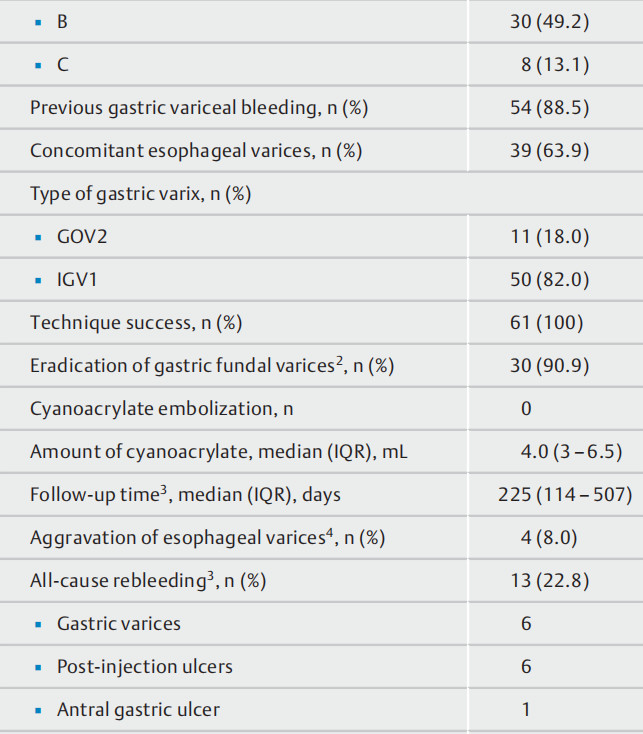
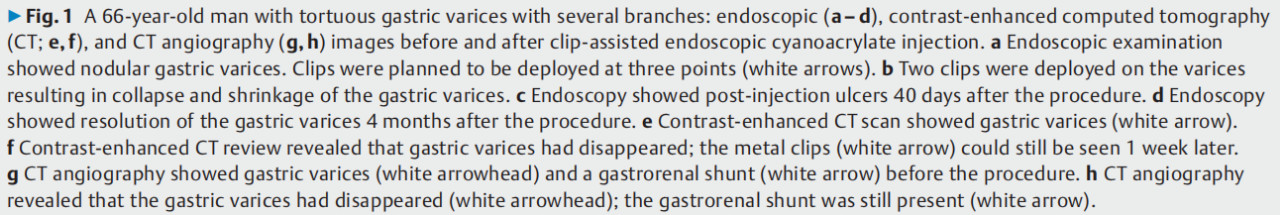
A total of 61 patients were analyzed in the study (see Fig. 1s in the online-only supplementary material). Patient characteristics are described in ?Table 1. The median follow-up time was 225 days (IQR 114 – 507 days), and four patients (6.6 %) were lost to follow-up.
Technical success rate
The clip-assisted endoscopic cyanoacrylate injection procedure was successfully performed in all 61 patients (100 %). Acute bleeding was immediately controlled in four patients, yielding a hemostasis rate of 100 %. A single metal clip was used in34.4 % of patients, two metal clips were used in 42.6 % of patients, and three or more metal clips were used in 23 % of patients. Reinjection of cyanoacrylate was performed in 36 patients during endoscopic surveillance. The reasons were inadequate filling of the varices. No adverse events occurred. A total of 50 patients underwent more than one endoscopy, and clips had completely fallen off in 18 patients during a median followup period of 108 days (IQR 101 – 200 days). The other applied clips remained on the gastric varices without forming any ulcerations. No bleeding was caused by shedding of the metal clips. No symptoms or signs of cyanoacrylate ectopic embolization related to the procedure were observed.
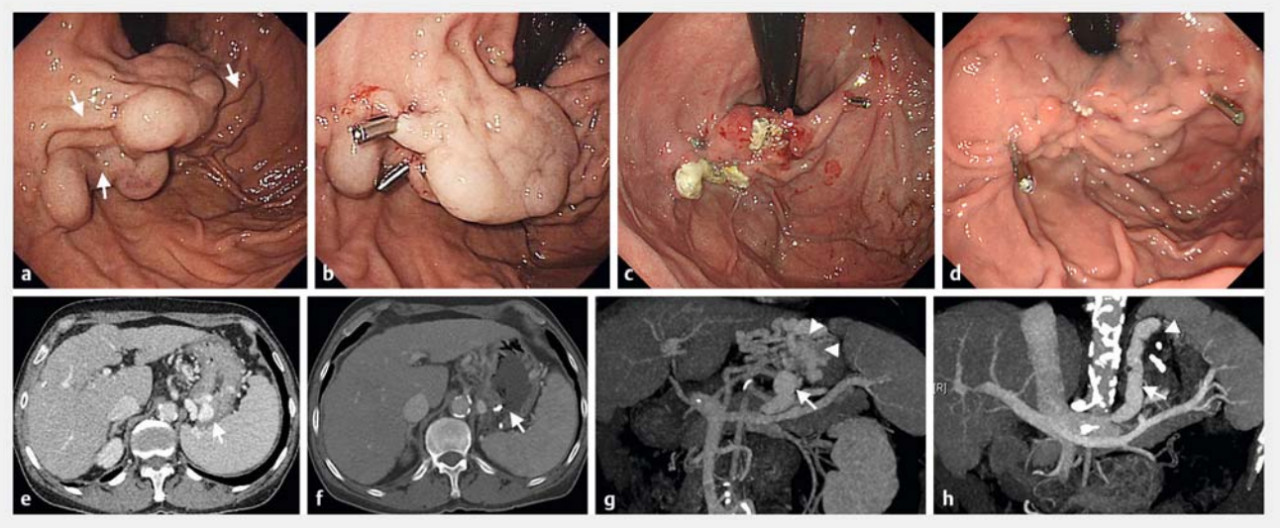
Eradication of gastric varices
Contrast-enhanced CT examination was performed on 33 patients within 1 month after the procedure. Gastric varices were eradicated in 30 of 33 patients (90.9 %) according to the contrast-enhanced CT re-examination.
Adverse events
One patient experienced transient variceal bleeding after a clip was deployed on the varix, and the bleeding was then controlled by cyanoacrylate injection (1 mL). Other mild adverse events were noted, such as fever and epigastric discomfort,which were relieved by symptomatic treatment. Endoscopic review was performed on 50 patients during a median time of 8days (IQR 7 – 34 days). Aggravation of esophageal varices occurred in four patients.
Rebleeding
During the follow-up period, all-cause gastrointestinal rebleeding occurred in 13 patients (22.8 %). Endoscopy was performed to determine the cause of rebleeding. Stigmata were found on the gastric varix in one patient and rebleeding was confirmed to be gastric variceal bleeding. In five patients with melena or hematemesis, no stigmata of bleeding were found, but there was also no bleeding source other than the gastric varices. Post-injection ulcers were found in six patients, and an antral gastric ulcer was found in one patient. Among the 13 patients, 2 patients underwent treatment with proton pump inhibitors and a vasoactive agent, and 11 patients underwent additional endo-scopic cyanoacrylate reinjection. Four patients required blood transfusion.
Discussion
Gastric variceal hemorrhage is associated with high mortality[2]. However, no global consensus has been reached regarding the optimal treatment, especially for bleeding from GOV2 and IGV1 varices [3, 8].
The clipping apparatus was originally developed to achieve endoscopic hemostasis of bleeding gastric ulcers and was further used for esophageal variceal bleeding [9]. Recently, Li et al. [10] reported endoscopic clipping prior to n-butyl-2-cyanoacrylate injection for one patient with bleeding attributable to gastric varices with a gastrorenal shunt. With this method,the inflow or outflow veins of the gastric varix were first clamped with metal clips to slow down or completely block the gastric variceal blood flow, followed by cyanoacrylate injection into the gastric varix. This novel approach may reduce the risk of ectopic embolization. To our knowledge, no report on a series of patients treated with this approach is available.
In our study, clip-assisted endoscopic cyanoacrylate injection was successfully performed in all 61 patients. No symptoms related to ectopic embolization were observed, reflecting an important difference from conventional endoscopic cyanoacrylate injection [11, 12]. Because neither cyanoacrylate nor lauromacrogol can be detected by X-ray, it was not clear whether asymptomatic ectopic embolization occurred. However, the group in this study had a gastrorenal shunt with a median diam-eter of 8mm, which places them at high risk for ectopic embolism. No symptoms related to ectopic embolization occurred. In a future study, a small amount of lipiodol should be added to the cyanoacrylate and non-contrast CT should be performed after the procedure to detect whether asymptomatic ectopic embolization has occurred. In the current study, gastric varices were eradicated in 30 of 33 patients (90.9 %) according to the contrast-enhanced CT re-examination. The rebleeding rate was22.8 % (13 of 57 patients), which is similar to that for conventional endoscopic cyanoacrylate injection [13, 14]. The results showed that this new method was safe and effective in the treatment of gastric varices with a gastrorenal shunt.
This study is the first reported series combining clips and cyanoacrylate to treat gastric varices with a gastrorenal shunt.The rationale for clamping the gastric varices was to slow down the blood flow rate of the gastric varices and thereby reduce the risk of cyanoacrylate embolization. The inflow veins,gastric varices, and outflow veins can be regarded as a whole blood flow channel. Regardless of whether the inflow or outflow veins are blocked, the blood flow within the gastric varices is restricted, thereby reducing the risk of ectopic embolization during cyanoacrylate injection.
This approach has several advantages. First, the procedure is convenient and easy to master, compared with both endoscopic ultrasound-guided endoscopic therapy and balloon-occluded retrograde transvenous obliteration-assisted endoscopic cyanoacrylate injection. Clip-assisted endoscopic cyanoacrylate injection does not require cooperation between endoscopists and interventional radiologists. Therefore, radiation exposure to both patients and doctors can be avoided. Second, no symptoms related to cyanoacrylate ectopic embolization were observed during the procedure. Additionally, the clips completely fell off in 18 patients during the follow-up period. No ulcerations caused by the clips occurred. The approach is safe for patients with a gastrorenal shunt, especially in reducing the risk of cyanoacrylate ectopic embolization compared with conventional endoscopic cyanoacrylate injection. Third,this approach is effective. The hemostasis rate for acute gastric variceal bleeding was 100 % in our study, and the rebleeding rate was similar to that for conventional endoscopic cyanoacrylate injection. No deaths were related to gastrointestinal bleeding.
The study has several limitations. First, the study was retrospective and therefore the possibility of selection bias cannot be excluded, although patients were screened according to the same inclusion and exclusion criteria across the three centres. Second, a control group was not available, although we did compare our results with those of previous studies of conventional endoscopic cyanoacrylate injection.
In conclusion, clip-assisted cyanoacrylate injection was convenient to perform and was safe and effective for treatment in patients with gastric varices combined with a gastrorenal shunt. In the future, prospective, randomized controlled clinical trials are warranted to compare this technique with other interventions.
References